Revitalizing Mobility: A Comprehensive Guide to Total Hip Arthroplasty and Hip Replacement
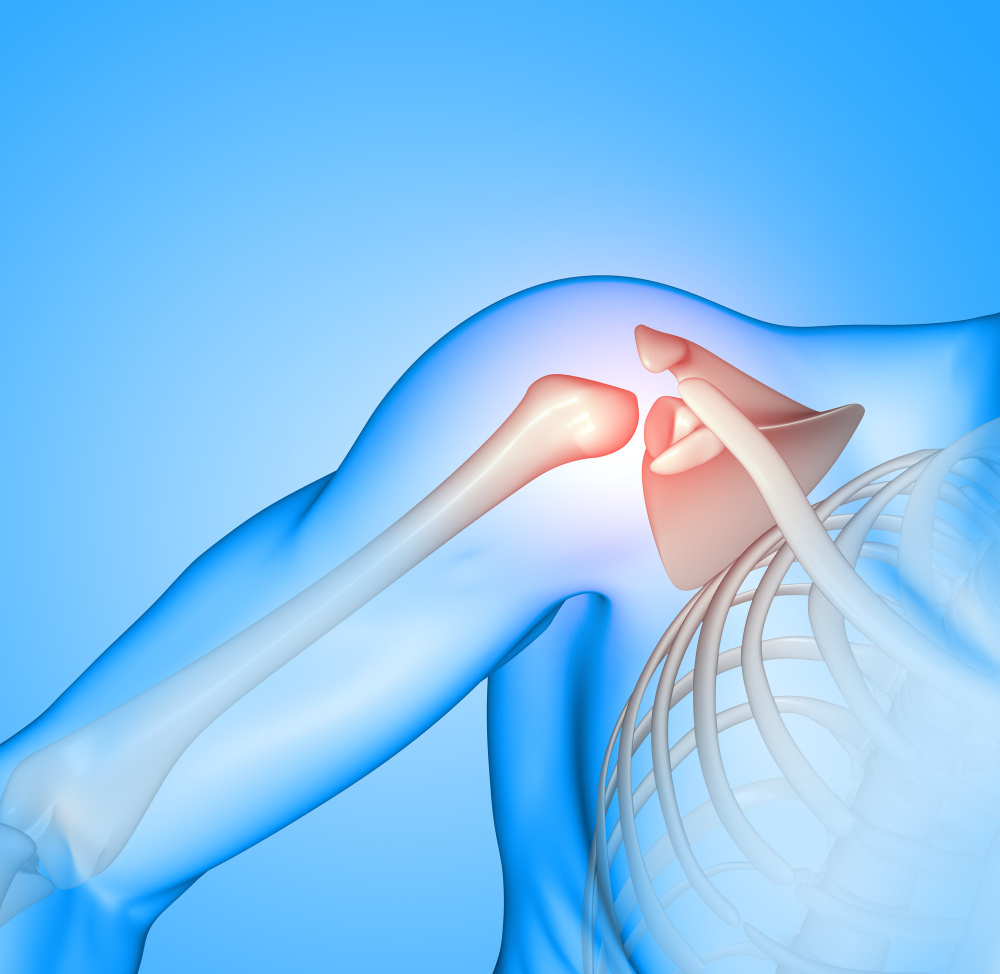
The human hip joint plays a pivotal role in our daily lives, facilitating movements from walking and sitting to more intricate actions. Unfortunately, conditions like osteoarthritis, rheumatoid arthritis, and fractures can compromise the hip joint, leading to pain, stiffness and diminished mobility. In such instances, medical advancements offer hope in the form of Total Hip Arthroplasty (THA), commonly known as hip replacement a surgical procedure designed to alleviate these issues and restore functionality to the hip joint.
As we delve into the world of Total Hip Arthroplasty, this blog aims to shed light on the transformative journey that individuals undergo—from the decision-making process and surgical nuances to the postoperative recovery and the restoration of a pain-free, active lifestyle.
Understanding Total Hip Arthroplasty (THA):
Total Hip Arthroplasty is a surgical procedure that involves replacing the damaged or diseased hip joint with a prosthetic implant. The procedure aims to relieve pain, improve hip joint function, and enhance overall mobility. It is often recommended for individuals with conditions like osteoarthritis, rheumatoid arthritis, or fractures that compromise the hip joint.
Key Stages of Total Hip Arthroplasty:
- Preoperative Assessment:
- Patients undergo a thorough evaluation to determine the extent of hip joint damage and assess overall health.
- Diagnostic imaging, such as X-rays and MRI scans, helps in planning the surgery.
Surgical Procedure:
- During the surgery, the damaged parts of the hip joint, including the femoral head and acetabulum, are removed.
- The prosthetic components, comprising a metal or ceramic ball and a socket, are then securely implanted.
- Recovery and Rehabilitation:
- Postoperative care involves a period of rehabilitation, including physical therapy, to regain strength and mobility.
- Patients are encouraged to gradually resume daily activities under the guidance of healthcare professionals.
Benefits of Total Hip Arthroplasty:
- Pain Relief:
THA effectively alleviates chronic hip pain, enhancing the overall quality of life for patients.
- Improved Mobility:
The restoration of the hip joint’s function allows for improved range of motion and enhanced mobility.
- Enhanced Quality of Life:
Patients often experience a significant improvement in their ability to perform daily activities and lead an active lifestyle.
Hip Replacement vs. Total Hip Arthroplasty:
While the terms are often used interchangeably, it’s crucial to distinguish between hip replacement and Total Hip Arthroplasty. The latter is a broader term encompassing various surgical techniques for hip joint reconstruction, including total and partial hip replacements. Hip replacement specifically refers to the complete replacement of the hip joint with a prosthetic implant.
Recovery and Rehabilitation:
Hip replacement recovery is a crucial phase in the patient’s journey towards restored mobility and improved quality of life. Understanding the recovery process is essential for individuals undergoing total hip arthroplasty (THA). Here’s an overview of key aspects related to hip replacement recovery:
- Immediate Postoperative Period:
Hospital Stay: Patients typically spend a few days in the hospital after surgery. During this time, medical professionals closely monitor vital signs, manage pain, and initiate physical therapy.
Mobility: Early mobilization, including standing and walking with assistance, begins soon after surgery to prevent complications like blood clots.
- Pain Management:
Medications: Pain management is a critical component of recovery. Patients are prescribed pain medications to alleviate discomfort during the initial stages.
Gradual Reduction: As the recovery progresses, the need for pain medication gradually decreases.
- Physical Therapy:
Range of Motion Exercises: Physical therapy plays a pivotal role in hip replacement recovery. Patients engage in range of motion exercises to enhance flexibility and prevent stiffness.
Strength Training: Progressive strength training exercises help build muscle around the hip joint, promoting stability.
- Weight-Bearing Activities:
Gradual Progression: Weight-bearing activities, such as walking with crutches or a walker, are gradually introduced.
Assistive Devices: Mobility aids are used initially and are phased out as the patient gains strength and stability.
- Home Recovery:
Assistance at Home: Upon discharge, patients may require assistance at home for activities like dressing, bathing, and preparing meals.
Home Exercise Program: Continued adherence to a prescribed home exercise program is crucial for sustained recovery.
- Return to Normal Activities:
Driving: The ability to resume driving is contingent on the individual’s progress and the type of surgery performed.
Work and Recreational Activities: Return to work and engagement in recreational activities are gradual processes, influenced by the patient’s overall health and the nature of their daily responsibilities.
Hip Replacement Risks.
While total hip arthroplasty (THA) is a highly successful and routine procedure, like any surgery, it carries certain risks and potential complications. It’s important for patients to be aware of these risks, although many individuals undergo hip replacement without experiencing major issues. Here are some potential risks associated with hip replacement:
Infection:
Risk: Infection is a potential risk with any surgical procedure. In the case of hip replacement, infections can occur at the surgical site or within the joint.
Prevention: Surgeons take precautions such as administering antibiotics before and after surgery to minimize the risk of infection.
Blood Clots:
Risk: Blood clots (deep vein thrombosis or DVT) can form in the veins of the legs. If a clot dislodges and travels to the lungs, it can cause a pulmonary embolism.
Prevention: Measures to prevent blood clots include the use of blood-thinning medications, compression stockings, and early mobilization.
Hip Dislocation:
Risk: There is a risk of the hip joint dislocating, especially in the first few weeks after surgery. This occurs when the artificial ball and socket are not properly aligned.
Prevention: Patients are advised to follow precautions, such as avoiding certain movements, to prevent hip dislocation.
Implant Wear and Loosening:
Risk: Over time, the artificial joint may wear down, and the components can loosen. This may necessitate a revision surgery.
Prevention: The choice of high-quality materials and proper surgical technique can contribute to the longevity of the implant.
Nerve and Blood Vessel Damage:
Risk: Injury to nearby nerves or blood vessels during surgery is a rare but possible complication.
Prevention: Surgeons take great care to minimize the risk of damage to surrounding structures.
Conclusion:
Total Hip Arthroplasty, commonly known as hip replacement, is a transformative surgical procedure that has provided countless individuals with relief from hip joint pain and restored their mobility. The decision to undergo THA is a collaborative process between patients and healthcare professionals, considering factors like overall health, lifestyle, and the severity of hip joint issues.
In conclusion, the journey from hip joint discomfort to the revitalization of mobility through Total Hip Arthroplasty is a testament to the advancements in medical science and the commitment to improving the lives of those affected by hip joint conditions.
FAQs-
Frequently Asked Questions (FAQs) about Total Hip Arthroplasty (THA) and Hip Replacement:
Q1: What is Total Hip Arthroplasty (THA)?
A1: Total Hip Arthroplasty, commonly known as hip replacement, is a surgical procedure where a damaged or diseased hip joint is replaced with an artificial joint or prosthesis. This is often performed to relieve pain and improve hip function.
Q2: When is Total Hip Arthroplasty recommended?
A2: THA is recommended for individuals experiencing severe hip pain, stiffness, and reduced mobility due to conditions like osteoarthritis, rheumatoid arthritis, or hip fractures that haven’t responded to conservative treatments.
Q3: How is the surgery performed?
A3: During THA, the damaged parts of the hip joint are removed and replaced with artificial components. The surgery can be performed using various approaches, such as posterior, anterior, or lateral, and may involve cemented or uncemented prosthetics.
Q4: What materials are used in hip joint implants?
A4: Hip joint implants are typically made of materials such as metal, ceramic, or polyethylene (plastic). Surgeons choose the materials based on factors like patient age, activity level, and potential allergies.
Q5: Can a hip replacement wear out, and how long do implants last?
A5: While hip replacements are designed to be durable, they may wear out over time. The lifespan of implants depends on factors like patient age, activity level, and the type of prosthesis used. On average, they can last 15-20 years or more.
Q6: Are there restrictions on activities after Total Hip Arthroplasty?
A6: Initially, patients may need to avoid high-impact activities. Over time, many can return to low-impact exercises. It’s essential to follow the surgeon’s advice on activity restrictions and modifications.
Q7: Can hip replacement surgery be performed on both hips simultaneously?
A7: While simultaneous bilateral hip replacement is an option for some patients, the decision depends on factors like overall health, age, and surgeon preference. Most often, surgeons perform the procedure on one hip at a time.

 Previous Post
Previous Post Next Post
Next Post