DAA-ARM Total Hip Replacement | Advanced Hip Surgery
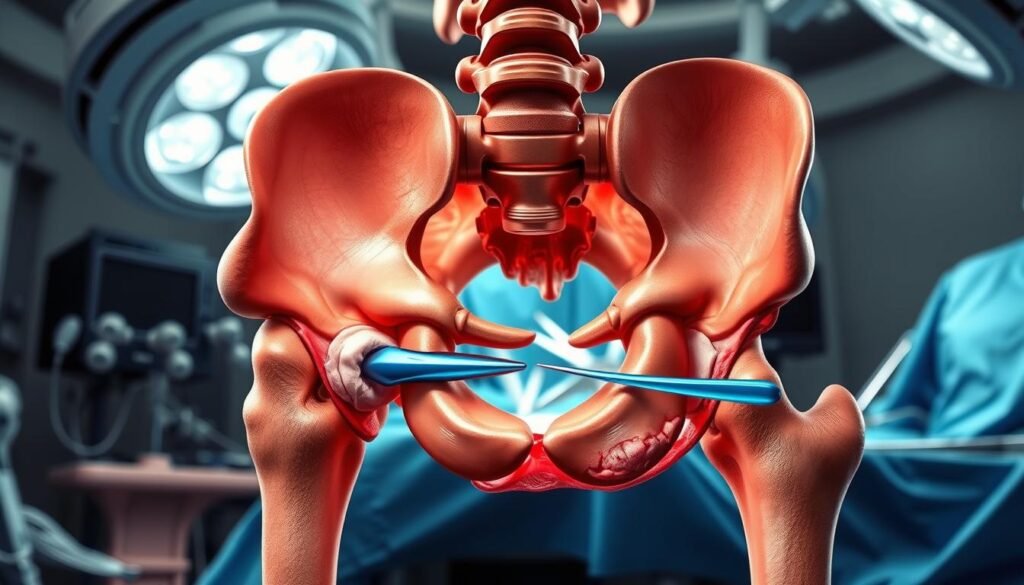
The direct anterior approach (DAA) to the hip has gained significant attention in recent years due to its tissue-sparing and minimally invasive characteristics.
This approach, initially described in the nineteenth century, has evolved to become a preferred method for total hip arthroplasty (THA). The DAA-ARM Total Hip Replacement represents a significant advancement in hip surgery techniques, combining the benefits of the Direct Anterior Approach with Advanced Reconstruction Methods.
By understanding the nuances of DAA-ARM, patients considering hip replacement surgery and surgeons looking to expand their technical expertise can make informed decisions.
Key Takeaways
- The DAA-ARM technique offers a minimally invasive approach to hip surgery.
- This method combines the benefits of the Direct Anterior Approach with Advanced Reconstruction Methods.
- DAA-ARM has gained popularity among orthopedic surgeons worldwide.
- The procedure covers the entire patient journey from candidate selection to rehabilitation.
- Understanding DAA-ARM is crucial for patients and surgeons alike.
Understanding DAA-ARM Total Hip Replacement
Understanding the nuances of DAA-ARM total hip replacement is crucial for patients considering hip replacement surgery. The Direct Anterior Approach with Acetabular and Femoral component Replacement (DAA-ARM) is a modern surgical technique that has gained popularity due to its muscle-sparing nature and reduced recovery time.
What is Direct Anterior Approach (DAA) Hip Replacement?
The Direct Anterior Approach (DAA) hip replacement is a surgical method that involves making an incision at the front of the hip to access the hip joint. This approach is considered muscle-sparing as it works between the muscles rather than detaching them from their insertions.
DAA hip replacement has been associated with several benefits, including reduced pain, shorter length of stay (LOS) in the hospital, lower dislocation rates, and faster recovery. The supine patient positioning during DAA-ARM surgery allows for more accurate assessment of leg length, offset, and component positioning using intraoperative fluoroscopy.
The Evolution of DAA-ARM Technique
The DAA-ARM technique has evolved significantly over the years, driven by advancements in surgical technology and a better understanding of hip anatomy. Initially developed as a modification of the traditional anterior approach, DAA-ARM has become a distinct method that combines the benefits of the direct anterior approach with advanced techniques for acetabular and femoral component replacement.
The evolution of DAA-ARM has been influenced by the desire to minimize tissue damage and promote faster recovery. As a result, DAA-ARM has become a preferred option for many orthopedic surgeons and patients seeking hip replacement surgery.
| Aspect | DAA-ARM | Traditional Approaches |
|---|---|---|
| Muscle Damage | Minimal | Significant |
| Recovery Time | Faster | Longer |
| Dislocation Rate | Lower | Higher |
Key Differences from Traditional Hip Replacement Approaches
DAA-ARM differs fundamentally from traditional posterior and lateral approaches in its muscle-sparing nature. While posterior approaches require detachment of the external rotators and posterior capsule, and lateral approaches disrupt the gluteus medius, DAA-ARM preserves these important muscle groups.
The differences between DAA-ARM and traditional approaches result in distinct post-operative precautions. DAA-ARM typically involves less restriction on hip positions compared to posterior approaches, where dislocation risk is higher.
Overall, DAA-ARM offers a promising alternative to traditional hip replacement methods, with potential benefits in terms of early recovery and reduced dislocation rates.
Benefits of DAA-ARM Total Hip Replacement
The DAA-ARM total hip replacement offers numerous benefits that have revolutionized the field of hip arthroplasty. This surgical technique has gained popularity due to its minimally invasive nature, reduced muscle damage, and improved stability.
Minimally Invasive Advantages
The DAA-ARM technique is characterized by its minimally invasive approach, which results in smaller incisions and less tissue damage compared to traditional hip replacement methods. This approach leads to reduced post-operative pain and a more aesthetically pleasing scar.
According to a recent systematic review with a meta-analysis, DAA THA resulted in significant reductions in the length of hospitalization, rate of dislocation, and overall postsurgical complication rate. The direct anterior approach allows for a more natural healing process, contributing to faster recovery times.
Reduced Muscle Damage and Faster Recovery
One of the key benefits of DAA-ARM is the reduced muscle damage associated with this technique. By using the intermuscular and internervous plane, the direct anterior approach minimizes the disruption of surrounding muscles and tendons, leading to less post-operative pain and a quicker return to normal activities.
Patients undergoing DAA-ARM typically experience a faster recovery due to the preservation of the posterior capsule and external rotators. This results in fewer position restrictions post-operatively, allowing for more natural movement patterns and potentially better functional outcomes.
| Benefits | DAA-ARM | Posterior Approach |
|---|---|---|
| Dislocation Rate | Lower | Higher |
| Muscle Damage | Reduced | More extensive |
| Recovery Time | Faster | Slower |
Lower Dislocation Rates and Improved Stability
The DAA-ARM technique is associated with lower dislocation rates compared to posterior approaches, attributed to the preservation of the posterior capsule and external rotators. Meta-analyses have consistently shown that DAA has a lower dislocation rate, which is particularly important for patients concerned about stability.
The improved stability profile of DAA-ARM means patients can typically return to normal sleeping positions and daily activities with less fear of dislocation, contributing to better quality of life during recovery. The technique allows for excellent visualization of the acetabulum, enabling optimal cup positioning, which is critical for joint stability and longevity.
Ideal Candidates for DAA-ARM Hip Surgery
Identifying suitable candidates for DAA-ARM hip surgery is essential for maximizing the benefits of this minimally invasive procedure. The Direct Anterior Approach (DAA) for hip arthroplasty has gained popularity due to its potential for reduced muscle damage and faster recovery times. However, not all patients are ideal candidates for this advanced technique.
Patient Selection Criteria
The selection of appropriate candidates for DAA-ARM hip surgery involves evaluating several key factors. These include the patient’s overall health, the severity of their hip condition, and their anatomical characteristics. Patients with a lower Body Mass Index (BMI) tend to have fewer wound complications, making them potentially better candidates. The direct anterior approach is particularly beneficial for patients who require a quick return to their normal activities.
Studies have shown that certain patient characteristics can influence the outcome of DAA-ARM hip arthroplasty. For instance, a study by Jahng et al found that diabetes mellitus was associated with an increased risk of wound complications following DAA total hip arthroplasty (THA). Therefore, careful perioperative glycemic control is crucial for diabetic patients undergoing this procedure.
Contraindications and Limitations
While DAA-ARM hip replacement offers several advantages, there are certain contraindications and limitations to consider. Patients with significant osteoporosis may be at a higher risk of intraoperative fracture during femoral preparation through the DAA-ARM approach. Additionally, individuals with a history of abdominal surgery with scarring near the anterior hip region may present challenges for the surgical approach and wound healing.
Pre-existing Conditions to Consider
Pre-existing conditions play a crucial role in determining a patient’s suitability for DAA-ARM hip surgery. Conditions such as inflammatory arthritis may complicate soft tissue considerations, potentially affecting healing and outcomes. Patients with neuromuscular conditions that affect gait and hip stability require careful evaluation. The presence of such conditions may necessitate adjustments to the surgical plan or postoperative care.
In conclusion, while DAA-ARM hip surgery offers numerous benefits, careful patient selection is paramount. By considering factors such as BMI, pre-existing medical conditions, and anatomical characteristics, healthcare providers can optimize outcomes for patients undergoing this advanced hip replacement technique.
Preparing for DAA-ARM Total Hip Replacement
The journey to a successful DAA-ARM total hip replacement begins with thorough preparation, which includes various assessments and lifestyle adjustments. Proper preparation is crucial for minimizing risks and ensuring a smooth recovery.
Pre-operative Assessments and Testing
Before undergoing DAA-ARM total hip replacement, patients are required to undergo comprehensive pre-operative assessments. These evaluations are designed to assess the patient’s overall health and identify any potential risks associated with the surgery. The assessments typically include:
- A thorough medical history review to identify any pre-existing conditions that could impact the surgery or recovery.
- A physical examination to assess the patient’s current physical condition, including gait, hip range of motion, and leg length.
- Imaging studies such as X-rays and MRI scans to evaluate the extent of hip damage and determine the most appropriate surgical approach.
These assessments are critical for developing a personalized surgical plan that addresses the patient’s specific needs and anatomy. By understanding the patient’s condition in detail, surgeons can better prepare for the procedure and anticipate any challenges that may arise during surgery.
Lifestyle Modifications Before Surgery
In the weeks leading up to DAA-ARM total hip replacement surgery, patients are often advised to make certain lifestyle modifications to optimize their health and reduce surgical risks. These modifications may include:
- Quitting smoking to improve circulation and overall health.
- Maintaining a healthy weight to reduce the strain on the hip joint.
- Engaging in gentle exercises to improve flexibility and strength.
By adopting these healthy habits, patients can potentially reduce their risk of complications and enhance their recovery process.
What to Expect During Consultation
During the initial consultation for DAA-ARM total hip replacement, the surgeon will perform a thorough physical examination, assessing gait, hip range of motion, and leg length. The consultation typically includes a detailed discussion of imaging findings, including the extent of arthritis, bone quality, and any anatomical considerations that might influence the surgical approach.
Patients should expect a comprehensive explanation of the DAA-ARM technique, including its potential benefits and limitations compared to other approaches based on their specific anatomy. The surgeon will discuss realistic expectations regarding recovery timeline, potential complications, and expected functional outcomes specific to the DAA-ARM total hip arthroplasty approach.
This consultation provides an opportunity for patients to ask questions about post-operative protocols, rehabilitation requirements, and when they can expect to return to specific activities following DAA-ARM surgery. By the end of the consultation, patients should have a clear understanding of what to expect and how to prepare for a successful hip arthroplasty outcome.
The DAA-ARM Surgical Technique
The DAA-ARM surgical technique represents a significant advancement in hip replacement surgery. This method combines the benefits of the direct anterior approach with specialized retraction techniques to minimize tissue damage and enhance recovery.
Patient Positioning and Setup
Proper patient positioning is crucial for the success of the DAA-ARM procedure. The patient is typically placed in a supine position on a specialized orthopedic table that allows for precise control over the hip joint. This positioning facilitates the direct anterior approach, enabling surgeons to access the hip joint with minimal muscle disruption.
Surgical Approach and Incision
The DAA-ARM technique involves a careful dissection through the interval between the tensor fasciae latae (TFL) and the sartorius muscle. After dissecting the subcutaneous tissue, the fascia of the TFL is scored, and the TFL is mobilized laterally. The branches of the lateral circumflex femoral artery are identified and cauterized just beneath the fascia using electrocautery. This meticulous approach helps in establishing the Heuter interval, which is crucial for accessing the hip joint.
Specialized Instruments and Equipment
The DAA-ARM technique requires specialized instruments, including retractors designed to gently retract the surrounding tissues without causing undue damage. These instruments are crucial for exposing the femoral neck and preparing it for osteotomy. The use of intraoperative fluoroscopy further enhances the precision of the procedure.
Step-by-Step Procedure Overview
The DAA-ARM procedure involves several key steps:
- The procedure begins with careful dissection through the TFL-sartorius interval, followed by identification and cauterization of the ascending branch of the lateral femoral circumflex vessels.
- After exposing the anterior hip capsule, a capsulotomy or capsulectomy is performed according to surgeon preference.
- The femoral neck osteotomy is performed in situ, with the exact level determined by preoperative templating and confirmed with intraoperative fluoroscopy.
- Following femoral head removal, specialized retractors are positioned to expose the acetabulum for preparation and component implantation.
- The femur is then externally rotated, extended, and adducted to expose the proximal femur for preparation and stem implantation.
| Step | Description | Key Considerations |
|---|---|---|
| 1. Dissection | Careful dissection through the TFL-sartorius interval | Identification and cauterization of lateral femoral circumflex vessels |
| 2. Capsulotomy/Capsulectomy | Exposure of the anterior hip capsule | Surgeon preference for capsulotomy or capsulectomy |
| 3. Femoral Neck Osteotomy | Osteotomy performed in situ | Preoperative templating and intraoperative fluoroscopy |
| 4. Acetabular Preparation | Exposure of the acetabulum | Use of specialized retractors |
| 5. Femoral Preparation | External rotation, extension, and adduction of the femur | Exposure of the proximal femur |
The DAA-ARM surgical technique offers a refined approach to hip replacement, leveraging the benefits of the direct anterior approach while minimizing tissue damage. By understanding the intricacies of this technique, surgeons can optimize outcomes for their patients.
Acetabular Component Placement in DAA-ARM Surgery
The precise placement of the acetabular component is a critical step in DAA-ARM total hip arthroplasty. This process involves several key steps and techniques to ensure optimal positioning and stability of the component.
Acetabular Preparation Techniques
Acetabular preparation is a crucial phase that precedes the placement of the final acetabular component. The bony bed is thoroughly cleaned with irrigation to remove any debris or residual cartilage. This step is essential for achieving a stable and secure fit of the acetabular component.
Key techniques in acetabular preparation include:
- Reaming the acetabulum to the appropriate size to accommodate the chosen acetabular component.
- Ensuring the acetabulum is properly positioned and aligned.
- Using trial components to check the fit before installing the final component.
Optimal Cup Positioning and Alignment
Optimal positioning and alignment of the acetabular cup are vital for the long-term success of the hip arthroplasty. Proper alignment helps in reducing the risk of dislocation and wear.
The use of intraoperative fluoroscopy plays a significant role in achieving optimal cup positioning. It allows the surgeon to visualize the position of the cup in real-time, making adjustments as necessary to ensure accurate placement.
Use of Intraoperative Fluoroscopy
Intraoperative fluoroscopy is a distinctive feature of DAA-ARM surgery, providing real-time imaging that enhances the accuracy of component positioning. For acetabular component placement, fluoroscopy helps confirm proper cup inclination, anteversion, and depth, reducing the risk of malposition that could lead to instability or impingement.
The C-arm is typically positioned to obtain anteroposterior pelvic views, with specific techniques to assess cup anteversion by measuring the degree of C-arm tilt required to see the cup as a line. Fluoroscopic guidance is particularly valuable during the learning curve of DAA-ARM surgery, providing immediate feedback and allowing for adjustments before final component seating.
The final acetabular component is placed under IOF C-Arm guidance after the bony bed has been cleaned with irrigation. The final component is installed, including the acetabular liner, and attention is turned to the femoral side.
Femoral Component Placement in DAA-ARM Surgery
The success of Direct Anterior Approach (DAA) total hip arthroplasty relies heavily on precise femoral component placement. This critical step in the surgical procedure requires a thorough understanding of femoral anatomy and the techniques involved in DAA-ARM surgery.
Femoral Exposure Techniques
Femoral exposure is a crucial initial step in femoral component placement. The direct anterior approach allows for minimally invasive exposure, reducing tissue damage and promoting faster recovery. Surgeons use specialized retractors to gently mobilize soft tissues, providing clear access to the femoral neck and shaft.
The use of intraoperative fluoroscopy aids in verifying the correct positioning of the femoral component. This real-time imaging helps surgeons make adjustments as needed to ensure optimal placement.
Femoral Preparation and Broaching
Once the femoral canal is accessed, the next step involves preparing the femur for component insertion. This includes broaching, where the surgeon uses progressively larger broaches to shape the femoral canal to match the chosen implant. The goal is to achieve a precise fit that supports the implant’s stability and longevity.
Component Insertion and Final Positioning
The final femoral component is inserted along the same path as the last broach, with careful attention to depth and rotational alignment. Trial components are used to assess stability, range of motion, and leg length before final implantation. Fluoroscopic imaging confirms proper component positioning, including stem alignment and the relationship between the femoral head center and the acetabular center of rotation.
The hip is reduced using controlled traction, internal rotation, and slight adduction. Stability is tested through a range of motion to ensure there is no impingement or tendency toward dislocation. The final assessment includes verification of leg length equality, offset restoration, and joint stability before wound closure.
Potential Complications and Risk Management
While Direct Anterior Approach (DAA) for total hip arthroplasty has shown numerous benefits, it’s crucial to acknowledge and manage potential complications associated with this technique. Effective risk management is key to achieving successful outcomes in DAA-ARM total hip replacement.
Common Complications Specific to DAA-ARM
DAA-ARM total hip arthroplasty, like other surgical procedures, comes with its own set of complications. Some of the common issues include infection, dislocation, and nerve injury. However, with proper preoperative planning and surgical technique, many of these complications can be minimized.
The direct anterior approach is associated with a unique set of potential complications, including lateral femoral cutaneous nerve injury and intraoperative fractures. Understanding these risks is crucial for their prevention.
| Complication | Description | Prevention Strategy |
|---|---|---|
| Lateral Femoral Cutaneous Nerve Injury | Nerve damage causing numbness or pain in the thigh | Careful dissection and nerve identification |
| Intraoperative Fracture | Fracture occurring during surgery | Preoperative planning, sequential capsular releases |
Lateral Femoral Cutaneous Nerve Injury Prevention
To prevent lateral femoral cutaneous nerve injury during DAA-ARM surgery, surgeons should employ careful dissection techniques and identify the nerve when possible. Understanding the anatomical variations of this nerve is also crucial.
Intraoperative Fracture Risk Reduction
Intraoperative fracture risk during DAA-ARM surgery can be reduced through careful preoperative planning, including assessment of bone quality and femoral morphology. Adequate femoral exposure through sequential capsular releases is essential to avoid excessive force during femoral preparation.
- Proper broach alignment parallel to the posterior femoral cortex helps prevent anterior perforation or calcar fractures.
- In patients with osteoporosis, consideration should be given to using tapered stem designs that require less aggressive broaching.
- Intraoperative fluoroscopy provides valuable feedback during femoral preparation, allowing for early detection and correction of potential fracture-inducing situations.
By understanding and addressing these potential complications, surgeons can improve the safety and efficacy of total hip arthroplasty using the DAA-ARM approach.
The Learning Curve for Surgeons

Mastering the DAA-ARM technique requires a comprehensive understanding and significant practice, underscoring the importance of a well-structured learning curve for surgeons. The Direct Anterior Approach for Total Hip Arthroplasty has gained popularity due to its minimally invasive nature and potential for faster recovery.
Training Requirements for DAA-ARM Proficiency
To become proficient in DAA-ARM, surgeons need specialized training that focuses on the nuances of the anterior approach. This includes understanding the anatomical landmarks and mastering the surgical technique to avoid complications.
Case Volume Needed for Mastery
The number of cases required to achieve mastery in DAA-ARM varies among surgeons. However, it is generally agreed that a higher case volume correlates with better outcomes and a reduced risk of complications. Surgeons transitioning from a posterior approach or lateral approaches should be prepared to invest time in practice.
Transitioning from Traditional Approaches
Surgeons transitioning to DAA-ARM from traditional methods face several challenges, including adapting to the Direct Anterior technique and understanding the different patient positioning. Collaboration with experienced surgeons and formal mentorship can significantly ease this transition.
Key considerations for surgeons include initially selecting ideal candidates with favorable anatomy, adopting a gradual transition approach, and understanding the differences in orientation and reference points in the supine position. Mastering femoral exposure and preparation techniques is also crucial.
Immediate Post-Operative Care
The immediate post-operative period following DAA-ARM total hip replacement is critical for managing pain and preventing complications. Effective care during this phase significantly influences the overall outcome of the surgery.
Pain Management Protocols
Pain management is a crucial aspect of post-operative care. Standard practice protocols allow for the injection of local anesthetic into the joint during surgery, which has been shown to provide good post-operative pain control. In the author’s experience, patients who underwent DAA-THA have demonstrated satisfactory pain management and are typically discharged within a day or two of surgery.
Multimodal pain management strategies are often employed, including the use of local anesthetics, NSAIDs, and other analgesics to minimize opioid use and their associated side effects.
Early Mobilization Strategies
Early mobilization is encouraged to prevent complications such as deep vein thrombosis and to promote recovery. Patients are typically advised to start moving shortly after surgery, with the help of physical therapists. The direct anterior approach for total hip replacement facilitates early mobilization due to its muscle-sparing nature, resulting in less tissue trauma and pain.
- Patients are encouraged to perform gentle exercises to maintain range of motion.
- Progressive weight-bearing activities are introduced gradually under the guidance of a physical therapist.
- Mobilization strategies are tailored to the individual patient’s needs and overall health status.
Wound Care and Monitoring
Wound care following DAA-ARM surgery is critical due to the incision’s location in the groin area, which is prone to moisture and friction. The anterior incision is typically closed with subcuticular sutures or staples and covered with a waterproof dressing that remains in place for 5-7 days.
Key aspects of wound care include:
- Monitoring for signs of infection, such as increasing redness, warmth, drainage, or systemic symptoms like fever.
- Avoiding excessive hip extension in the early healing phase to minimize tension on the wound.
- Keeping the wound dry and clean, with the waterproof dressing aiding in this process.
By following these guidelines for immediate post-operative care, patients who have undergone DAA-ARM total hip replacement can expect a smoother recovery process, with reduced risk of complications and improved outcomes.
Rehabilitation After DAA-ARM Total Hip Replacement
After undergoing DAA-ARM surgery, patients enter a comprehensive rehabilitation program tailored to their needs. The goal of this program is to optimize functional recovery and enhance patient satisfaction following total hip replacement.
The rehabilitation process after DAA-ARM total hip replacement is divided into three phases, each with specific objectives and exercises designed to promote healing and restore function.
Phase 1: Initial Recovery (0-2 Weeks)
During the initial recovery phase, the focus is on managing pain, reducing inflammation, and improving mobility. Patients are encouraged to perform gentle exercises such as ankle rotations, isometric contractions, and short walks.
Early mobilization helps prevent complications like deep vein thrombosis and promotes healing of the hip arthroplasty.
Phase 2: Progressive Mobility (2-6 Weeks)
In the second phase, patients progress to more challenging exercises, including straight leg raises, hip abductions, and gradual strengthening of the surrounding muscles. Progressive resistance training is introduced to enhance strength and stability.
Functional exercises such as direct anterior approach-specific movements are incorporated to improve flexibility and range of motion.
Phase 3: Advanced Strengthening (6+ Weeks)
The advanced phase of rehabilitation focuses on restoring normal strength, endurance, and function for return to desired activities. Progressive resistance training incorporates weights, resistance bands, and more challenging body weight exercises to build strength in the hip abductors, extensors, and rotators.
Functional exercise progressions include lunges, step-ups/step-downs, and multi-directional movements that mimic daily activities and recreational pursuits. Cardiovascular conditioning becomes more emphasized, with stationary cycling, elliptical training, and progressive walking programs to build endurance.
Sport-specific or activity-specific training may be introduced for patients wishing to return to golf, tennis, hiking, or other recreational activities, with appropriate modifications based on individual goals and abilities.
Expected Outcomes and Recovery Timeline
Patients considering DAA-ARM total hip replacement often ask about the expected recovery timeline and outcomes. The direct anterior approach has gained popularity due to its minimally invasive nature, leading to faster recovery times and improved patient satisfaction.
Short-term Recovery Milestones
In the initial weeks following DAA-ARM total hip replacement, patients typically experience significant progress. Most patients can return to light work, such as desk jobs, within 2-4 weeks after surgery. More physically demanding occupations may require 6-12 weeks of recovery. Low-impact recreational activities like walking, swimming, and stationary cycling can usually be resumed by 6 weeks, with gradual progression based on comfort and confidence.
Long-term Functional Outcomes
The direct anterior approach is associated with improved long-term functional outcomes due to reduced muscle damage during surgery. Studies have shown that patients who undergo DAA-ARM hip replacement often experience better functional recovery, enabling them to return to their daily activities with greater ease.
As patients progress in their recovery, they can expect to see continued improvement in their functional abilities. This is largely due to the precise nature of the DAA-ARM technique, which allows for more accurate component placement and optimal soft tissue management.
Return to Daily Activities and Sports
Patients are often eager to return to their favorite sports and activities after total hip replacement. Golf is generally permitted around 6-8 weeks, starting with putting and chipping and progressing to full swings as comfort allows. Higher-impact activities like tennis, hiking on uneven terrain, and dancing can usually be resumed by 3-4 months with appropriate technique and conditioning.
While there are no absolute restrictions after healing is complete, most surgeons advise permanent avoidance of extreme high-impact activities like running marathons or contact sports to maximize implant longevity. This guidance is crucial for ensuring long-term patient satisfaction and functional recovery.
As highlighted by a study on DAA-ARM outcomes, “The direct anterior approach for total hip arthroplasty has been shown to result in excellent functional outcomes and high patient satisfaction rates.” This quote underscores the effectiveness of the DAA-ARM technique in achieving positive results for patients.
Comparing DAA-ARM with Other Hip Replacement Approaches
The direct anterior approach (DAA) and other methods for total hip arthroplasty have distinct advantages and potential complications. Understanding these differences is crucial for optimizing patient outcomes and making informed decisions about the most appropriate surgical technique.
DAA vs. Posterior Approach
The DAA and posterior approach are two commonly used techniques for total hip arthroplasty. Studies have compared these approaches to determine their relative benefits and drawbacks. A meta-analysis by Ang et al. found that the DAA was associated with improved early functional outcomes and a shorter mean length of stay compared to the posterior approach. However, the DAA was also associated with a longer operative time.
Key differences between DAA and posterior approach:
- DAA typically results in less pain in the first 2-6 weeks post-operatively.
- Posterior approach has a higher risk of dislocation.
- DAA may have a higher risk of lateral femoral cutaneous nerve injury.
DAA vs. Direct Lateral Approach
The direct lateral approach is another technique used for total hip arthroplasty. Comparing the DAA to the direct lateral approach reveals differences in complication profiles and recovery outcomes. Randomized controlled trials have shown that DAA patients tend to have less pain and faster recovery in the early post-operative period.
Evidence-Based Outcome Comparisons
Systematic reviews and meta-analyses provide valuable insights into the comparative outcomes of different surgical approaches for total hip arthroplasty. A systematic review of 11 randomized controlled trials found that the DAA resulted in comparable functional recovery to the posterior approach. The evidence suggests that while there are differences in early recovery and complication profiles, long-term functional outcomes tend to be similar across approaches.
| Surgical Approach | Early Recovery | Complication Profile | Long-term Outcomes |
|---|---|---|---|
| DAA | Faster recovery, less pain | Higher risk of LFCN injury, early femoral fractures | Comparable to other approaches |
| Posterior Approach | Slower recovery, more pain | Higher risk of dislocation | Comparable to other approaches |
| Direct Lateral Approach | Variable recovery | Higher risk of nerve injury, muscle damage | Comparable to other approaches |
In conclusion, while the DAA and other surgical approaches for total hip arthroplasty have different benefits and risks, the evidence suggests that surgeon experience and comfort with a given approach may be more important than the specific technique used.
DAA-ARM Total Hip Replacement in India

Schedule Your Consultation Today
India has emerged as a hub for advanced medical procedures, including DAA-ARM total hip replacement. The country’s healthcare sector has made significant strides in adopting innovative surgical techniques like the Direct Anterior Approach for total hip arthroplasty.
Availability and Adoption in Indian Hospitals
The availability of DAA-ARM total hip replacement is increasing in major Indian cities, with several top hospitals now offering this advanced procedure. Patients seeking this surgery can find specialized care in hospitals that have adopted the latest hip arthroplasty techniques.
High-volume centers performing at least 100 hip replacements annually are more likely to have surgeons proficient in DAA-ARM and the necessary specialized equipment.
Cost Considerations and Insurance Coverage
One of the significant advantages of undergoing DAA-ARM total hip replacement in India is the cost-effectiveness. The procedure is often more affordable compared to many Western countries, making it an attractive option for medical tourists.
Many Indian insurance providers now cover total hip arthroplasty procedures, including DAA-ARM. Patients are advised to check with their insurance providers for specific coverage details.
Finding Specialized Surgeons in India
To find a qualified surgeon for DAA-ARM hip replacement, patients can look for professionals who have completed specialized fellowship training in the technique, preferably with international experience.
Professional orthopedic societies in India, such as the Indian Orthopaedic Association, can provide referrals to surgeons with expertise in advanced hip replacement techniques.
Advancements and Future Directions in DAA-ARM Technology
Advancements in DAA-ARM technology are revolutionizing the landscape of hip replacement surgery. The Direct Anterior Approach for total hip arthroplasty has seen significant improvements in recent years, enhancing patient outcomes and expanding the possibilities for surgeons.
Robotic-Assisted DAA Surgery
One of the most significant advancements is the integration of robotic assistance in DAA surgery. Robotic systems provide surgeons with enhanced precision, allowing for more accurate implant placement and better outcomes in Total Hip Arthroplasty procedures. This technology is particularly beneficial in complex cases, where the precision offered by robotic assistance can significantly impact the success of the surgery.
Navigation Systems and Precision Tools
Navigation systems and precision tools are also playing a crucial role in the evolution of DAA-ARM technology. These systems enable surgeons to achieve optimal component positioning, which is critical for the longevity and functionality of the hip arthroplasty. By utilizing advanced navigation, surgeons can reduce the risk of complications and improve patient recovery times.
Emerging Research and Innovations
Ongoing research is exploring several promising areas, including the integration of artificial intelligence with intraoperative imaging to provide real-time guidance during DAA-ARM procedures. Novel implant designs optimized for the anterior approach are being developed, featuring modified geometries that facilitate easier insertion. Enhanced recovery protocols specific to DAA-ARM are being refined through systematic research to accelerate rehabilitation and improve outcomes. Wearable technology for post-operative monitoring is also being studied to track recovery metrics and provide early warnings of potential complications.
| Innovation | Description | Benefit |
|---|---|---|
| Robotic-Assisted Surgery | Integration of robotic systems for enhanced precision | Improved accuracy in implant placement |
| Navigation Systems | Advanced tools for optimal component positioning | Reduced risk of complications |
| Artificial Intelligence | Real-time guidance during DAA-ARM procedures | Enhanced surgical precision |
As research continues to advance, the future of Hip Arthroplasty looks promising, with potential improvements in patient care and surgical outcomes. Long-term outcome studies comparing DAA-ARM to other approaches will provide valuable data on implant longevity and patient satisfaction over decades, contributing to a systematic review and meta-analysis of the most effective techniques.
Conclusion
DAA-ARM represents a cutting-edge approach in hip arthroplasty, enhancing patient outcomes through its minimally invasive technique and advanced reconstruction methods. This surgical approach has garnered significant attention in the field of orthopedic surgery due to its potential benefits, including early recovery, reduced muscle damage, and lower dislocation rates.
The Direct Anterior Approach (DAA) is a key component of DAA-ARM, offering a tissue-sparing advantage that contributes to the overall success of the procedure. By combining DAA with advanced reconstruction methods, surgeons can optimize component positioning and improve functional outcomes for patients undergoing Total Hip Arthroplasty.
One of the critical factors in the success of DAA-ARM is patient selection. Ideal candidates typically have a BMI under 30, favorable hip anatomy, and no significant deformities. However, experienced surgeons can adapt the technique for more complex cases, making it a versatile option for a wide range of patients.
The learning curve for DAA-ARM is substantial, requiring approximately 50-100 cases for a surgeon to achieve proficiency. Despite this challenge, surgeons who master the technique can provide excellent results, highlighting the importance of specialized training and experience in Total Hip Replacement surgery.
Post-operative rehabilitation after DAA-ARM benefits significantly from the muscle-sparing nature of the approach. Patients can typically expect earlier mobilization and fewer restrictions compared to traditional hip replacement methods, contributing to a smoother and more rapid recovery.
As technology continues to evolve, the integration of robotic assistance, navigation systems, and specialized instrumentation is likely to further enhance the precision and reproducibility of DAA-ARM. This ongoing innovation will play a crucial role in shaping the future of Hip Arthroplasty and improving patient outcomes.
For patients considering hip replacement, it is essential to discuss with their surgeon whether DAA-ARM is appropriate for their specific condition, anatomy, and goals. While the technique offers numerous benefits, the experience and expertise of the surgeon are critical factors in determining the success of the procedure.
In the Indian context, DAA-ARM is becoming increasingly available in major medical centers, providing patients with access to this advanced technique and its potential benefits for accelerated recovery. As the availability of DAA-ARM continues to grow, it is likely to become a more prominent option for patients undergoing Total Hip Arthroplasty in India.
Contact By Dr. Aniket Patil :
At Om Hip & Knee Specialty Orthopedic and Physiotherapy Clinic in Kharadi, Pune, led by Dr. Aniket Patil — a fellowship-trained orthopedic and joint replacement surgeon — we specialize in advanced treatments including DAA-ARM Total Hip Replacement and comprehensive orthopedic care. With extensive experience and modern surgical techniques, our clinic provides personalized hip replacement solutions designed to improve mobility, reduce pain, and restore quality of life. We proudly serve patients from Pune, Pimpri-Chinchwad (PCMC), Hadapsar, Viman Nagar, Wagholi, and surrounding regions, offering compassionate care in a supportive, patient-focused environment.

 Next Post
Next Post